BLOG
Levi's Surgery Story
The biggest unexpected surprise for our family came in July of 2016, when we took Levi in for a routine physical exam prior to having his teeth cleaned. Dogs have to go under anesthesia to have their teeth cleaned, and Levi has traditionally had some issues related to anesthesia and we wanted to be safe. His last checkup was in April 2016; he went in for an ear infection and at that time, he was in perfect health (except for the ear infection, of course). So it came as quite a shock when the vet announced that he heard a heart murmur level 4/5 for the first time in Levi's life...
Kim, Ginny, and Levi. Photo taken by Carolyn Scott Photography
The biggest unexpected surprise for our family came in July of 2016, when we took Levi in for a routine physical exam prior to having his teeth cleaned. Dogs have to go under anesthesia to have their teeth cleaned, and Levi has traditionally had some issues related to anesthesia and we wanted to be safe. His last checkup was in April 2016; he went in for an ear infection and at that time, he was in perfect health (except for the ear infection, of course). So it came as quite a shock when the vet announced that he heard a heart murmur level 4/5 for the first time in Levi's life.
A lot of small dogs develop a gradual heart murmur that starts low and builds as the dog gets older. We would not have been surprised if, at 9 years of age, that Levi had a minor heart murmur. But to go from zero murmur in April to a level 4/5 in July is alarming.
Heart murmurs in dogs can occur for many reasons, but the most typical of which is degenerative mitral valve regurgitation. The mitral valve is a flap in the heart that allows blood to pump into the ventricle, but not backwards towards the lungs. As a valve should work, it allows one-way movement. Degenerative mitral valve disease causes the thickening of the valve to the point at which it does not close properly and blood moves back and forth ineffectively in the heart. In response, the heart enlarges to allow for a larger capacity of blood pooling and to keep blood pressure in the body stable. Eventually, the excess fluid will back up into the lungs causing congestive heart failure.
We went to the cardiologist at the earliest possible moment. He confirmed that Levi did indeed have a level 5 murmur caused by degenerative mitral valve disease exacerbated by a chordae tendonae rupture. There are chords in the heart (literally what country singers croon about when they sing about heartstrings) that help coordinate the movement of the mitral valve flaps. If they break, the effectiveness of the valve is compromised significantly. That explains why it was not a gradual increase in murmur grade, but all at once.
We were devastated by the news, and we were further shocked when we were told that Levi had 6-9 months before he experienced congestive heart failure, and possibly a year left to live. We left with this news heavy in our hearts. Our devastation turned to anger and frustration. Why is there nothing that anyone can do to correct this issue in dogs? Humans have open heart surgery to repair the heart valves all the time - it's practically routine!
We emailed veterinarians at UC Davis, Cornell University, and several other highly respected veterinary schools in the US, along with one point of contact we found for veterinary surgeons in France. We heard back from the French doctors - they asked for more information about Levi and his results from our cardiologist.
We sent them, and held our breath.
We found more information about the doctors in France, and other dogs and owners from the US who had gone there to have the repair done. We called. We coordinated. We kept researching. No veterinary team in the US performs this procedure. Only one surgeon in the world - renowned Japanese surgeon named Dr. Masami Uechi - performs these operations currently in Japan, Singapore, and France.
Levi was in the loving care of Dr. Jean-Hugues Bozon and Dr. Sabine Bozon during his surgery and recovery
When we finally got word from the Clinique Veterinaire Bozon in Versailles, France that Levi was a candidate, we were still in a little bit of disbelief that this was possible, that this was actually something that we could and possibly WOULD do. Were we crazy? Would other people think we were crazy? Can we logistically pull this off?
Maybe we are crazy, maybe we just love our dog. We stopped caring what anyone thought of what we were doing. And yes, we logistically pulled it off . . . one day at a time, one piece at a time, one foot in front of the other. When you want to do something that seems impossible in foresight (and hindsight), you have to know that the little steps in between to make it happen just come as long as you keep moving. We never lost faith, even when it was tested over and over again. I was taught that my heart and my hope are infinitely bigger than I ever realized.
It was unexpected. All of it. The diagnosis. The plan of action. Even the result.
Levi with Dr. Neal Peckens at CVCA
We expected resistance and judgement anytime we talked about cardio-pulmonary bypass surgery for our dog . . . in FRANCE. But, everywhere we turned, friends and family knew exactly what Levi meant to us, and agreed we were doing the right thing for him. Our vets Dr. Carole Richards and Dr. Chris Vanderhoof at Caring Hands Animal Hospital, and Dr. Neal Peckens at CVCA, were 100% on board with us when we made the decision to go forward with it. They ran tests, and re-ran tests, and asked questions, and cared for us as owners. They cheered us on, and helped Levi recover when we got back.
We knew before we even went to France for the surgery, before we even knew Levi would live through it, that we wanted to be of service to Dr. Sabine and Jean-Hugues Bozon. We didn't know how, but we felt so inspired by what they are doing. When we met them, saw their clear vision of the future, learned about the many leaps of faith they took to get where they are, and witnessed the loving care they put into every living being that they touch, it was very clear to us and a few owners who came before, that we would need to take our own leap of faith to help them, and to help this cause in some way. And that is one of many reasons that Mighty Hearts Project was born.
Though most of all, it was unexpected what two people with love and hope in their hearts can accomplish together. I do mean Ginny and myself; however, we saw it in Dr. Sabine and Jean-Hugues as well. Their love for each other and their love for saving animals is unparalleled. Dr. Sabine taught us not to ever lose faith in something that is important to you. If the solutions presented to you are unacceptable, find new solutions.
We are currently on a mission to find new solutions for dogs in the United States. We will not lose faith.
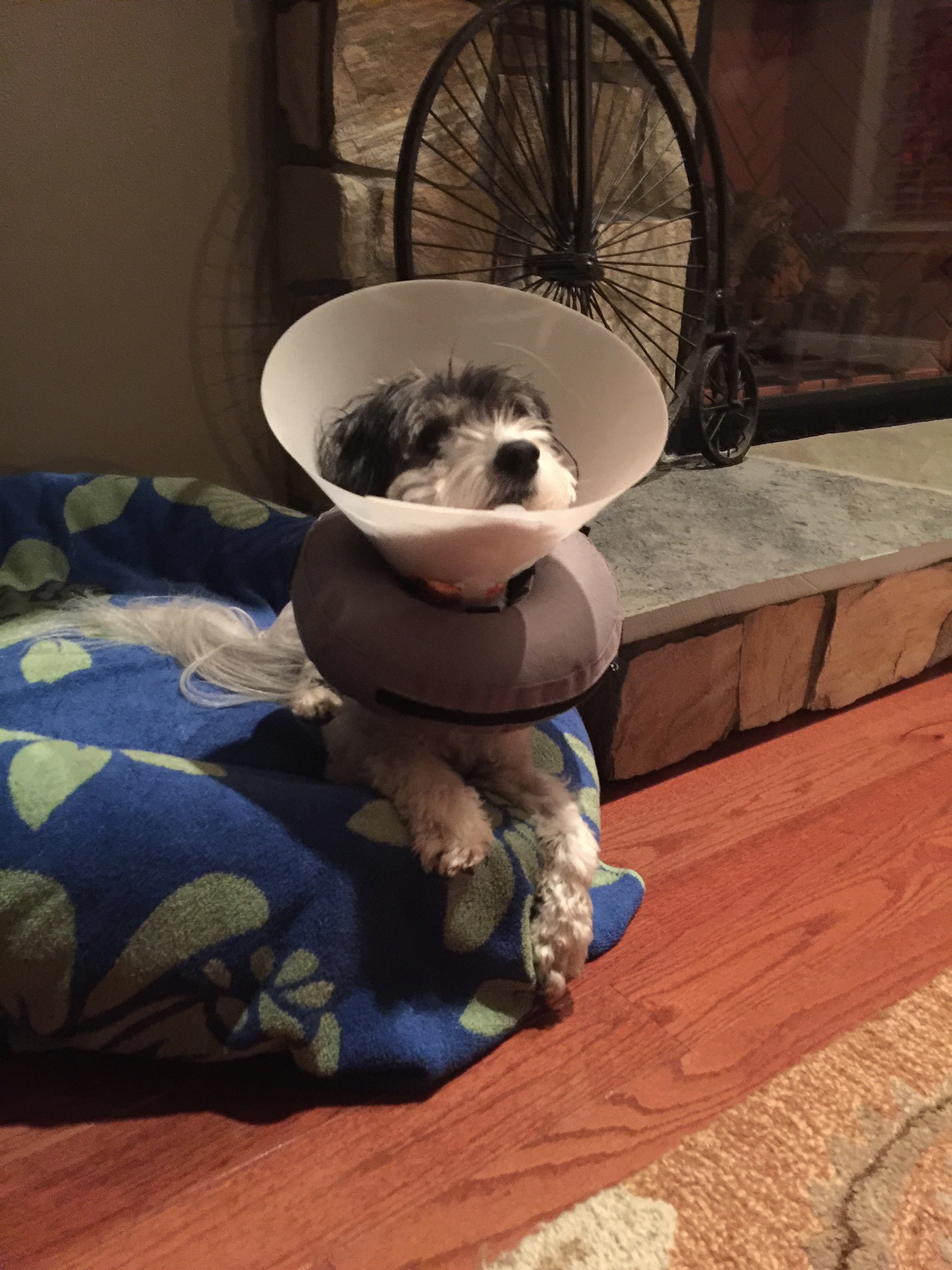
Levi, sitting up in his oxygen recovery cage just a few hours after his mitral valve repair surgery at Clinique Veterinaire Bozon in Versailles, France
The LOOK Study: ACVIM Conference 2017
The Longitudinal Outcome of Canine Mitral Valve Disease (LOOK-mitral) - by Dr. Michele Borgarelli, DVM, PhD, DECVIM-CA
This is a study being performed with the collaboration of Virginia-Maryland College of Veterinary Medicine, where Dr. Borgarelli does his research, and one of the largest veterinary cardiology practices in the United States, CVCA. The purpose of the study is to assess the natural history of mitral valve disease (MVD) in a large referred population of dogs, assess the prevalence and effects of co-morbidities on the natural history of the disease, and to identify risk factors for progression and death.
The Longitudinal Outcome of Canine Mitral Valve Disease (LOOK-mitral) - by Dr. Michele Borgarelli, DVM, PhD, DECVIM-CA
This is a study being performed with the collaboration of Virginia-Maryland College of Veterinary Medicine, where Dr. Borgarelli does his research, and one of the largest veterinary cardiology practices in the United States, CVCA. The purpose of the study is to assess the natural history of mitral valve disease (MVD) in a large referred population of dogs, assess the prevalence and effects of co-morbidities on the natural history of the disease, and to identify risk factors for progression and death. Collected data includes physical exam, radiographic findings, ECG findings, presence of co-morbidity, laboratory results and treatments.
Since October 2015, vets from CVCA have been submitting information from a large population of dogs with MVD to the LOOK Study. This is strictly an observational study. Inclusion criteria for study enrollment is a diagnosis of MVD confirmed by echocardiographic exam. Dogs are enrolled in the study at the time the diagnosis is confirmed by a cardiology specialist. 2,053 dogs have been observed as of April 30, 2017, and new dogs can continue to be submitted to the study until September 2017. Data on the dogs enrolled in the study will continue to be collected until it concludes in October 2020 or until the death of the dog.
The current population of dogs in the study represent 104 different breeds. The largest segment being mixed breed at more than 300 dogs, second highest is CKC, then Chihuahua. 48% of dogs are female, and 52% are male, and for both male and female, approximately 90% are neutered/spayed. The median age of all dogs is 10.3 years, but it was noted that the average age for the CKC is much younger than the median.
57% are Stage B (75% of which are B1, 25% are B2), 39% are Stage C, and 4% are Stage D. During the current 20 months of the study, only 4.5% of dogs have passed. It was noted that this could be because most dogs being submitted to the study were new cases presented at CVCA which typically occur at the earlier stages.
Some of the preliminary findings of the study so far are:
- Echocardiogram results are more important than the observation of a heart murmur, as more than 4% of dogs with the disease had zero murmur. In high risk breeds, this suggests that regular preventative cardiology exams with echocardiogram are warranted rather than waiting until the onset of symptoms.
- Nearly 80% of dogs are referred to cardiologists due to the presence of a cough.
- Most concomitant disease is chronic respiratory disease.
Additionally, at the conclusion of the conference session, Mighty Hearts Project participants were able to inquire with Dr. Borgarelli on whether dogs who have had an intervention, such as Dr. Uechi's Mitral Valve Repair surgery, were noted and being tracked within the study with this information in mind. Dr. Borgarelli confirmed that is correct. One dog that we know of being tracked as part of the LOOK study is Levi, who has had a successful mitral valve repair since his initial diagnosis. Levi is seen by Dr. Neal Peckens at CVCA in Virginia.
Bellissima's Surgery Story
This is our big story of one small cute girl and the big love between us forever.
We have had Bellissima (Belisa) from the very first day she was born because we also were parents to her mummy. She has three siblings which were all given to our friends so that they would be in good hands. We also had new parents for Belisa, but we felt that we belonged to each other so we kept her.
“This is our big story of one small cute girl and the big love between us forever.
—Tomáš Kučera”
We have had Bellissima (Belisa) from the very first day she was born because we also were parents to her mummy. She has three siblings which were all given to our friends so that they would be in good hands. We also had new parents for Belisa, but we felt that we belonged to each other so we kept her.
She is typical terrier, excited about everything, angry at everybody, and so much energy - crazy like a puppy. We had to have her spayed because she was suffering from false pregnancy (or pseudopregnancy). She was mothering her toys and having problems with her mammary glands. Our doctor told us that after being spayed, Belisa would be calmer and not so interested in sex with her toys… but that was not true at all. She wanted to have sex with everything and was even crazier than before.
After that she started to limp on her left back leg and was diagnosed with a luxating patella. We found a specialist from Croatia, Dr. Dokič, who gave her a titan implant in her leg. Unfortunately she had to have an additional operation because the titan implants are made of two pieces and they split up. She also had a groin hernia which was the first time we saw her crying in pain. She had never cried in pain before that.
In 2014, she had her first epileptic seizure. We were shocked because at that time we didn’t know about epilepsy in dogs. We read a lot of information about epilepsy and learned that there is no true cure. We finally decided not to visit doctors who would only give her drugs and scare her more. Every time a seizure was coming she came to us and let us know that something was happening to her, so that we could hold her, talk to her, and try to distract her from what was happening, which worked quite well.
Also in 2014, our doctor told us that she had a heart murmur but it was nothing to worry about. We didn’t know any better and believed our doctor. In October 2015, Belisa was put on Vetmedin (Pimobendan) and Furosemide. Again, our doctor told us there was nothing to worry about. In August 2016, we were visiting our doctor and he told us everything was still fine.
In December 2016, our doctor told us that Belisa was getting worse. Of course, we thought, because she had started to cough during the night and we didn’t understand why. We asked him how much time she has left and his answer killed us. 6 – 12 months. He told us that there was one person in the world that might be able to help us, Dr. Uechi, but it's too expensive. Nothing is too expensive if our love has just a few months of life left. We didn’t know the price, but we knew that we could sell our flat, our cars, our company, even my kidney, anything, just to save her life.
We googled Belisa's condition and Dr. Uechi, and thanks to Kaori and her story of Ralph, we found this amazing group of selfless people. Of course we didn’t believe or understand why there is only one person in the world who could help us. It seemed so strange to us. So in January, we flew to France to meet Dr. Sabin Bozon to discuss the surgery and assess whether we were doing the right thing. We have never ever met a doctor this kind. She is an angel. She explained everything to us and spent a lot of time emailing us answers to all of our questions. This was the most helpful thing during this time, when you are losing all hope.
We did all the tests in our country, including magnetic resonance because of Belisa's epilepsy, to ensure that her brain was fine, and then we had to decide whether to do her surgery in March or May. We knew the risk of the surgery (every surgery is a risk, of course, however, this is not like her leg, it's her heart!), and preferred May. However, we decided to take Belisa to visit Dr. Sabine so that she could see Belisa and give us better advice about when to do the surgery. We selfishly wanted May, but this was not about what we wanted, it was about what Belisa needed.
Dr. Sabine gave us advice to go in March because she was not sure if Belisa would stay stable until May. She told us during that visit that there was another problem called Myocardial thinning, which is another risk with Degenerative Mitral Valve Disease. She gave us another type of medication for Belisa. From that visit until the surgery we were giving her multiple medications at specific times of the day. We were very tired because some of them were very late in the evening, some of them very early in the morning, and most of the time during the night we were not sleeping because we were checking on her to see if she was fine and still breathing.
On March 17, Belisa had her last recheck with Dr. Sabine and she told us that all the numbers of the tests were much better. On March 21, the day of surgery, I told Belisa in the morning that we belong to each other; we will stay together forever no matter what. We will be waiting for you in the front of clinic, be strong girl, we know you will come back to us. I am certain she understood us.
If Marla, Michael, and Dominique were not also at the clinic in the days after Belisa's surgery, we would have just sat quietly for the whole time of post-care (which is seven days normally, and we paid for one extra day to be sure) in the car in front of the clinic. Car? Yes, the journey to France by plane takes about 1.5 hours, but we went by car so that Belisa could go pipi anytime she needed to and she wouldn't be as scared of all the people.
After waking from anesthesia post-surgery, Belisa had some problems with breathing because she also has a collapsing trachea. Even today her breathing is not 100% better, but I am sure it will get better. Dr. Sabine explained to us that an enlarged right ventricle is not as life threatening as the left side. The left side is already smaller after the surgery. The right side will get slightly bigger and it will take some time, but it will get smaller again.
Our journey back home was also not easy. We left France at 1:30 am because we knew Belisa would be calmer at night. When we were about 400km from France, and 600km from our home, Belisa started to cry and kept her right back leg (the healthy one) up. We turned the car around and drove back to Dr. Sabine. She gave Belisa some drugs for pain and we started our journey again.
When we arrived home, she was not able to walk normally. Even the front leg was bad. Today, we don’t know exactly what happened to her (all the doctors we spoke to about it have different ideas – orthopedic, spinal, neurologist etc.), but she is now walking almost like normal and we are sure it will just take some time to be 100% good.
This is our big story of one small cute girl and the big love between us forever.
Mitral Valve Repair Metrics
One of the most frequent questions asked when considering a surgery as risky as cardio-pulmonary bypass, is what are the chances my dog will survive the surgery and what is the long term prognosis post-surgery. The answer is always "it depends". Each dog is different, and each circumstance is unique. Below are some guidelines to help you determine the best course of action for your dog based on aggregate data. For more specific recommendations regarding surgery for your dog, please contact Clinique Veterinary Bozon or JASMINE Veterinary Medical Center directly. Additional mitral valve repair statistics may be found in an abstract published by Dr. Masami Uechi from October 2016.
One of the most frequent questions asked when considering a surgery as risky as cardio-pulmonary bypass, is what are the chances my dog will survive the surgery and what is the long term prognosis post-surgery. The answer is always "it depends". Each dog is different, and each circumstance is unique. Below are some guidelines to help you determine the best course of action for your dog based on aggregate data. For more specific recommendations regarding surgery for your dog, please contact JASMINE Veterinary Medical Center directly. Additional mitral valve repair statistics may be found in an abstract published by Dr. Masami Uechi from October 2016.
Global survival rates of dogs who have undergone Mitral Valve Repair with Dr. Masami Uechi:
99% in stage B2
95% in stage C (if no pulmonary hypertension (PHT) before surgery)
85% in stage C (if there is PHT before surgery)
75% in stage D
The younger the dog is, the higher the success rate.
80% of the dogs operated on do not need any treatment or additional medications for mitral valve disease after surgery.
Mitral valve repair is needed if one or more of these conditions are present:
If the dog is 13 years old or less AND
As soon as the dog is in stage C
If there is chordae tendinae rupture and/or grade 3 prolapse (even in stage B2)
If there is a grade 3 or 4 mitral regurgitation (even in stage B2)
If pulmonary arterial pressure (PAP) is less than 50 mmHg (otherwise the dog must be put on sildenafil 1-2 months before surgery)
If the 2D LA/AO ratio in SAX is > 1.6 (right parasternal) (The LA/AO - meaning Left Atrial to Aorta Ratio - uses the relatively fixed diameter of the aorta to assess the degree of left atrial volume loading)
If the NT-ProBNP level is > 2100 mol/l (even in stage B2)
Mitral Valve Repair under Cardio-Pulmonary Bypass (CPB) is a very complicated procedure
Weak points triggering a poor recovery from CPB are:
The age of the dog (older dogs are more prone to Systemic Inflammatory Response Syndrome and thrombosis after surgery because their endothelium is more damaged)
The degree of PHT before surgery (because one of the side effects of CPB is PHT)
The systolic/myocardial function (because there is myocardial ischemia during CPB and the recovery is directly related to the myocardial health before surgery)
The severity of the ACVIM stage
The surgery might be contraindicated (or have a lower survival rate) if:
The dog is more than 13 years old
There is severe PAP not improved after sildenafil therapy
There is myocardial dysfunction/ischemia (low cardiac output) before surgery
There is any concomitant medical disease (a secondary illness), for example:
A neoplastic process (a mass or tumor)
everely impaired renal function such as nephrotic syndrome or protein-losing enteropathy (kidney disorders)
Severe hepatic insufficiency (liver failure)
Unresolved infections
ndocrine disease (such as Cushings)
Hypothyroidism can be adjusted and treated 2-3 months before surgery
There is coagulation dysfunction (an issue with blood clotting) and especially decreased levels of antithrombin 3 before surgery
Surgery might be difficult if there is a significant aortic insufficiency, an observation that must be recorded in the cardiology report
Post-Surgical Strategies for Restricting Activity
Whether your dog has undergone Mitral Valve Repair surgery, or any number of other surgeries that require a period of activity restriction in order to recover, it can be difficult to control their energy level and normal habitual activities. Here are some strategies for success.
Whether your dog has undergone Mitral Valve Repair surgery, or any number of other surgeries that require a period of activity restriction in order to recover, it can be difficult to control their energy level and normal habitual activities. In addition to the strategies outlined below, please read the additional guidance for activity levels beyond the 3-month post-operative period here.
Many owners wonder "why is activity restricted after Mitral Valve Repair surgery?"
The surgery involves an open-heart element which needs time to heal. In addition, there are many carefully placed sutures inside the heart along the valve to complete the annuloplasty – the purse-string stitch that tightens the opening of the valve – and the replacement Gore-Tex heart cords attached to the valve and left ventricle. In most cases, the efficacy of these sutures depends on the quality of healing time without being under too much unnecessary pressure.
If your dog has undergone Mitral Valve Repair surgery, activity is restricted significantly for the three months post-operative. This includes no running, jumping, stairs, or any activity that gets them too excited. For a dog that just underwent a procedure that will make them feel like a puppy again, restricting their energy is a tough job. Here are some strategies to consider.
Prepare your environment at home:
- Take the doorbell off the hook and put a note on the door that knocking is strictly prohibited.
- Block off any stairs up or down in the house.
- Block off the edge of furniture items if your dog typically jumps up without invitation.
- Invest in a lightweight movable/re-configurable gate structure that can be placed anywhere.
- Put away all toys that your dog may spontaneously play with.
- Build or invest in a pet ramp so they can walk, not jump, onto furniture items they typical sit and sleep on.
For extra control, and for dogs who are not trusted to roam freely:
- Make sure your dog stays with you in whatever room of the home you are in and keep doors closed to limit roaming.
- Consider a leash (non-retractable) used with a simple collar or harness over a sweater or onesie to avoid direct contact with the incision site. Using the leash, maintain a short lead while on furniture if your dog is prone to jumping down on their own, and a long lead to tie your dog to various furniture items on the floor to keep them from wandering around.
- Use a lightweight gate structure or crate to keep them contained especially when you are not at home or while you are asleep.
Natural remedies:
- There is a natural supplement called Zylkene which has a calming effect in some dogs. The effect is cumulative, and should be given for at least a week consistently to achieve the desired effect. All dogs react to supplements differently, this product works very effectively for some, and not at all for others. You can take comfort that Zylkene is totally natural and will not harm your dog, and cannot be overdosed.
- Use a sound or "white noise" machine to create ambient noise so your dog does not overreact to typical noises outside the house that they might normally bark or get excited at or go tearing through the house to investigate, especially when you are not at home.
Upon discharge from the clinic, you will be provided with post-operative instructions for activity for your dog for a period of three months. These instructions are intended to keep your dog’s blood circulating and to help slowly recondition them so they can return to normal activity levels in three months. The current guideline post-operative for the first month is 15 minutes of slow walking, 4 times per day. This is intended to be the absolute maximum for the most active dogs and also much lower than your dog’s regular activity level. Throughout the three month recovery period, the doctors will advise when it’s appropriate to increase the amount of time walking and at what suggested interval levels.
For those who have yet to go through Mitral Valve Repair surgery, some of these suggestions may seem a little extreme for a three month period. Some dogs can suffer from some mild depression when restrained for extended periods and it can be difficult to stay strong for them. However, taking precautions and following the doctor’s discharge notes on exercise ensures that you are giving your dog the best possible chance to heal and get the maximum benefit from surgery.
Traveling With Home Prepared Meals
Traveling by air internationally with your dog can be a stressful event. If you home cook for them, preparing fresh meals can also be difficult. Some accommodations may not have full kitchens and finding the same ingredients that you typically use can also be challenging in a foreign country. This article will help you bring your dog’s prepared frozen food with you as a carry on while still complying with the Transportation Security Administration’s (TSA) security checkpoint rules.
Traveling by air internationally with your dog can be a stressful event. If you home cook for them, preparing fresh meals can also be difficult. Some accommodations may not have full kitchens and finding the same ingredients that you typically use can also be challenging in a foreign country. This article will help you bring your dog’s prepared frozen food with you as a carry on while still complying with the Transportation Security Administration’s (TSA) security checkpoint rules. The following guidelines are from the TSA’s website and additional details can be found here.
“Meat, fish, vegetables, and other non-liquid food items are permitted in both carry-on and checked bags. If the food is packed with ice or ice packs in a cooler or other container, the ice or ice packs must be completely frozen when brought through screening. If the ice or ice packs are partially melted and have any liquid at the bottom of the container, they will not be permitted.
Even if an item is generally permitted, it may be subject to additional screening or not allowed through the checkpoint if it triggers an alarm during the screening process, appears to have been tampered with, or poses other security concerns. The final decision rests with TSA on whether to allow any items on the plane.”
I successfully traveled with my dog’s frozen food by using the Igloo MaxCold Duffle Cooler shown below. This product is relatively inexpensive and available at many online retailers and local stores such as Target or Walmart. I also purchased a few gel icepacks and brought a few freezer bags with regular ice to ensure the gel ice packs didn’t melt on the way to the airport. Before going through the checkpoint I removed the freezer bags of ice, leaving the frozen gel ice packs in the bag. I informed the TSA security agents of the contents of my bag and that it was my dog’s food and necessary because she has severe food allergies. I passed through security and onto my flight. My food was still completely frozen even when I arrived at my hotel to store it in the freezer.
Here are some tips and tricks to ensure you have no issues getting your food to your final destination – and what to do if for any reason you cannot.
When dumping your ice at the airport, which keeps your gel icepacks frozen solid for TSA checkpoint clearance, keep the zip lock bags. They can be refilled on the airplane with ice from any of the flight attendants. This is especially helpful if for any reason your gel icepacks have melted and are not permitted beyond the security checkpoint.
If there is room in your checked luggage, you can put the entire cooler with food and ice packs in that and there will be no issues with TSA, even if the ice packs do start to melt. It does take up quite a bit of room though.
Make sure your final destination has an adequate freezer. If you are staying at a hotel that doesn’t have a freezer or fridge, check to see if they have ice makers in the building so that you can refresh your zip lock bags once or twice a day with cold ice. You may also contact the front desk to see if you can use an employee freezer.
There are several days directly after surgery where your dog will most likely not be fed your home made food while hospitalized. The doctors at each clinic will let you know when you can bring your own food for your dog during the hospital stay. If you don’t want them to use standard commercial foods it would be a good idea for you to bring your own and get the approval to do so.
Article written by Nate Estes, featuring Zoey Marie Estes
Zoey's First MVR Surgery Story
Zoey was diagnosed with Mitral Valve Disease (MVD) in July of 2016.
We were told it was a disease of the heart where the valve degenerates causing a regurgitation of blood back into the heart, ultimately leading to congestive heart failure and death. They said nothing surgically could be done to fix this, only medication to delay its onset.
As you can imagine we were devastated, left without any hope. Zoey was only given a year left to live...
Zoey was diagnosed with Mitral Valve Disease (MVD) in July of 2016.
We were told it was a disease of the heart where the valve degenerates causing a regurgitation of blood back into the heart, ultimately leading to congestive heart failure and death. They said nothing surgically could be done to fix this, only medication to delay its onset.
As you can imagine we were devastated, left without any hope. Zoey was only given a year left to live.
I searched frantically online for something and found that Cornell University hosted a team of Japanese doctors that perform Mitral Valve Repair surgery. Dylan Raskin was able to secure the funds to fly them to the US, hotel them and cover all the medical expenses.
His dog Esme was almost at death's door but two years after this surgery is more than saved, she healthy and like a puppy.
Sadly, the doctors are only performing this surgery in France, Japan, and Singapore and are the only ones qualified in the world doing the surgery. I learned all I can about this and in the end, I flew my dog from Los Angeles to France for an open-heart mitral valve repair surgery.
The surgery was done October 26th 2016 by Dr. Masami Uechi and Jean Hugues Bozon of the Clinique Veterinaire BOZON 2424 in Versailles France.
Zoey is healing well and her heart has already reduced in size.
Her energy level is like a puppy. Zoey is off Pimobendan and Enalapril for good. She only requires blood thinners for the first three months of recovery to avoid blood clots. No running or jumping as well until cleared by Dr. Sabine Bozon who is Zoey's cardiologist in France. In addition to her work Dr. Sabine also does the Pre-operative patient profiling and is the director of the surgical aftercare program for her clinic.
Prior to surgery, Zoey's heart was extremely large and her left atrium vein was dilated and stretched.
The surgery also revealed she was almost going to have a chord rupture. Once this is healed, her heart will continue to shrink and her murmur should reduce as well.
Our three-month post-op check is on January 28th with Dr. Hodge from UC Davis's satellite office in San Diego. Zoey's surgery had no complications and was expected to have a 98 percent result. We feel truly blessed with the level of care we have received from the 6 day ICU care from the Bozon clinic.
Currently, no US surgeon is able to perform this surgery unless they'd study abroad learning Dr. Masami's technique, bringing it back to the US.
The surgery involves heart and lung bypass machine (seen in pics) which the Bozons are the only certified specialists outside of Japan qualified to do small animal bypass.
It involves strengthening the mitral valve with a gortex loop and reattaching the valve to the heart wall with six gortex chords to replace the stressed or stretched out chords. In addition, they strengthen and add extra chords to the heart to ensure any possible future ruptures will have no ill effects on the condition.
The goal of this surgery is to restore them to the B1 stage and repair the valve as much as possible to reduce the regurgitation.
By using the gortex material, there is no rejection. Valve replacements have been attempted yet failed because the body rejected it. Anti-rejection medications didn't work.
This surgery is currently the only option to save dogs suffering from MVD and most cardiologists are unfamiliar with it.
This is history in the making.
I am always asked about the cost and why is it so expensive so here it is. The clinic is using state of the art medical equipment that most human hospitals dream of having, such as the mentioned cardiopulmonary bypass machine and a cell saving machine that allows for a transfusion of Zoey's own blood during surgery should she have needed it. Donor blood is also available onsite in the case more is needed.
I didn't have the money but was able to secure high-interest rate loans that I barely could afford. I did this without hesitation to save Zoey.
God bless,
Nathan Estes