BLOG
Zoey Marie's Second MVR Surgery
I wanted to share the actual second mitral valve repair surgery of my brave daughter Zoey Marie Estes.
I wanted to share Zoey’s second mitral valve repair surgery video. Thank you to Dr. Masami Uechi, Sayaka Takeuchi, Ayaka Chen and the entire Jasmine team for your unbelievable dedication towards saving my daughters life not once but twice. You all have saved so many lives of dogs suffering with mitral valve disease and for that we are forever grateful and hold you all dearly in our hearts. Below is Zoey’s brave second journey story.
Zoey’s second surgery journey
Just after two years since having her first mitral valve repair surgery in France by Dr. Masami Uechi and the Bozon’s team we noticed Zoey was again progressing from this dreadful disease at each checkup things kept looking different. I was actively working with the clinics in France and Japan to understand what was going on with Zoey to cause this. After a few difficult months of piecing it together we realized Zoey may have torn a major artificial chordae that was placed during her first surgery in France in 2016.
Proactively I already started the Japanese quarantine process which is a six-seven month waiting period proving rabies immunity before you are allowed to enter the country. We found ourselves yet again facing the possibility of doing another bypass repair surgery on Zoey, otherwise she probably wouldve only had a year left to live as she was already moving towards congestive heart failure (CHF), she was only seven years old now.
So we prepared for Japan per Masami Uechi’s request. The day came to embark on our second mitral valve repair journey, this time a different continent. Much like the first, we were prepared for what lies ahead. We arrived a week early to acclimate Zoey and had our pre-op surgical appointment with the wonderful Sayaka Takeuchi. We were faced with the scary truths about the risks involved in this second surgery and needed to make a heavy decision on whether we would again proceed. Obviously with Zoey quickly advancing and knowing the road that was ahead we placed our unwavering faith in Dr. Masami Uechi and his team and our faith in god and decided to proceed ahead to save our little daughter again.
We were told second surgeries were rarely performed and they weren’t even sure on how successful it could be. They were not sure why this happened to Zoey as it’s not very common unless a dog was to active early on in the recovery process causing a chordae to detach before allowing them the required three months time to scar and bond over the repair to the heart further reinforcing the repair. Was it a weak heart muscle or stress we will never know. All I know is here we are again faced with the same fears a little over two years ago.
Surgery day came and I won't lie that I was a complete wreck internally, outwardly I was holding it all together for my family that needed me to be the rock. As they took Zoey away from me yet again, a wave of calmness went through my body because I knew I gave Zoey’s little body the best chances at fighting this again and I knew the team cared deeply about us and would save my daughters life again, I had no doubts in my soul.
Surgery started, sitting again in that lobby, knowing my daughter was clinically dead for the second time was the most difficult thing I had to witness for the second time in my life. As you sit in the lobby you find yourself reading each doctors reactions as they come and go gauging how it’s going inside the surgical room. It’s such a heart-wrenching feeling. Sitting in the lobby waiting and seeing how many more dogs are coming in to be examined as future patients is devastating and makes you realize how much of a problem this disease is worldwide.
Finally
Dr. Masami Uechi comes out to bring you back to the surgical theater to explain to you how it all went “heart sinking” he tells us all went as planned and Zoey is off the bypass machine and being closed up by the team. As Dr. Uechi shows us the repair results we are crying in relief and amazement of what this beautiful man and team just did again saving our daughter.
We are lead to the back of the room to see Zoey being stitched up and Dr. Uechi is explaining what the vital signs on the monitor means, blood pressure, heart rate, etc. We are thrilled yet worried as the recovery is just as crucial as the surgery. They did their job and now Zoey’s body and the recovery team start theirs. What a roller coaster and miracle.
As Zoey was moved to recovery and we were able to see, I again had to be the rock holding us all together to see her through this. As the days went on we strengthened Zoey with proper nutrition to get her numbers to improve from the natural bodies inflammation response to this intervention. Zoey did remarkably well and eventually was able to check out of the clinic and come back to our Airbnb. She did have to go back to the clinic a few times and the amazing team at the Jasmine clinic were able to get Zoey’s numbers yet again stabilized.
Headed home
Zoey persevered through all the obstacles against her for the second time and we got to go home. After a much needed rest at our home in the US, we went for our checkup with Dr. Emily Chapel at Access Specialty Animal Hospital and she was so impressed with how well Zoey was doing since the last time she saw Zoey before going to Japan for surgery. You always find yourself at each cardiologist appointment holding your breath because we’ve been here before and you never know what they are going to say in the future towards this progressive disease.
It’s been quite a life-changing journey for us and the immense support from the Mighty Hearts MVD Community was just amazing and a remainder of why I helped to create and continue to maintain this important resource. This experience has only further strengthened my determination at dedicating my life to this cause to save more of our babies lives and to continue helping all the families get through this as gently as possible. Mighty Hearts Project needs all of you working together with us for the common cause of advancing this procedure all over the world.
One thing I’ve learned is just how important it is for us to support these doctors learning this surgery. As they make it more readily available throughout the world, we must advocate for them in doing this procedure in the proper manner increasing the lives saved as they all advance in these emerging programs. I truly hate this disease and my resolve is strong to continue to grow our organization towards helping all of those we support. It won’t be perfect and I’m sure many bumps will happen along the way. To learn is to grow and sometimes letting the path lovingly guide you to where it needs you is what I’ve learned.
My little daughter is alive and inspiring myself and many others along the way to never quit in life until your soul is needed elsewhere. I love all of you and and will never quit in my resolve to seeing you all through your difficult journey’s to hopefully come home with your babies on the other side of this terrible disease.
Lessons From Zoey's One Year Checkup
Zoey’s one year checkup was done October 28th 2017. Zoey’s cardiologist (Dr. Hodge) was a bit worried Zoey’s left ventricle and left atrium (LV/LA) numbers were increasing after each checkup. According to Dr. Hodge, Zoey’s pressure and her regurgitation were shown to be the same since having her surgery a year ago. Naturally We were concerned about the increasing values and sent the records off to Dr. Sabine and Dr. Uechi to review them.
UC Davis Veterinary Medical Center in San Diego, CA
Zoey’s one year checkup was done October 28th 2017. Zoey’s cardiologist (Dr. Hodge) was a bit worried Zoey’s left atrium and left ventricle (LA/LV) numbers were increasing after each checkup. According to Dr. Hodge, Zoey’s pressure and her regurgitation were shown to be the same since having her surgery a year ago. Naturally We were concerned about the increasing LA/LV values and sent the records off to Dr. Sabine and Dr. Uechi to review them.
Dr. Timothy Hodge evaluating Zoey
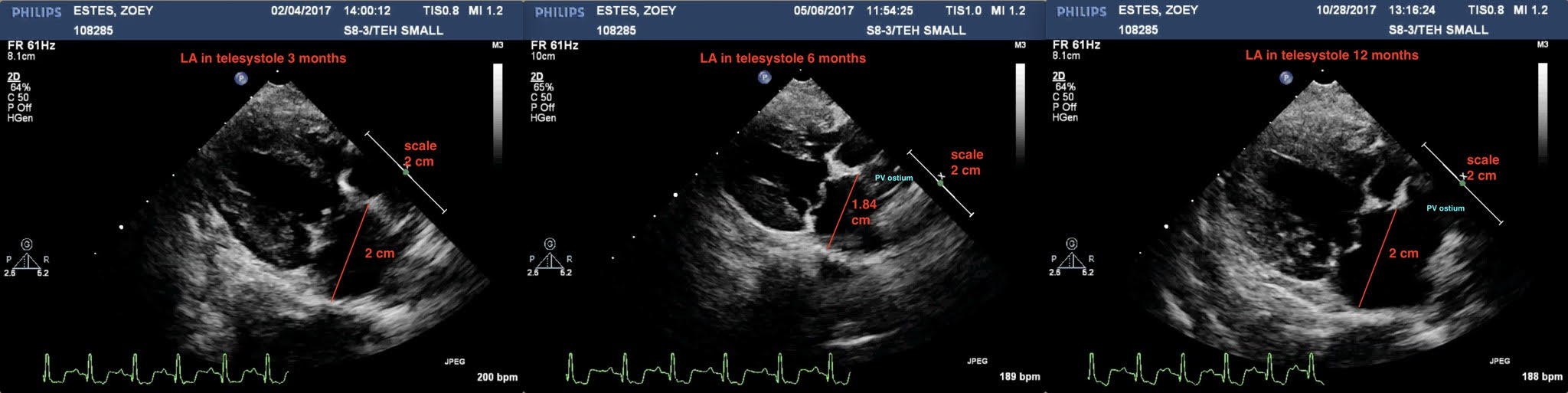
I’m delighted to say that It was great news. Dr. Sabine and Dr. Uechi compared Zoey’s numbers from her surgery echos to her 3, 6 and one year checkups and the values appeared to be the same since she had her surgery in 2016. It was extremely important for me to learn exactly why it was being seen differently with my doctor and share with you all what I’ve come to learn.
Basically Zoey has a larger than normal pulmonary vein (ostium) since before her surgery and standard measuring practices can give false numbers if you don’t account for these results.
According to Dr. Sabine, the 1st reconstruction is of the Long axis LA diameters in telesystole at 3-6-12 months. Measured 2, 1.84 and 2 cm, basically they are the same measurements ; the SAX measurements are somehow difficult with Zoey because she has a very large pulmonary vein ostium compared to other dogs. As noted, (Zoey had this before her MVR surgery)
Echocardiograms showing Left Atrium (LA) measurements at 3 months, 6 months, and 12 months post operatively
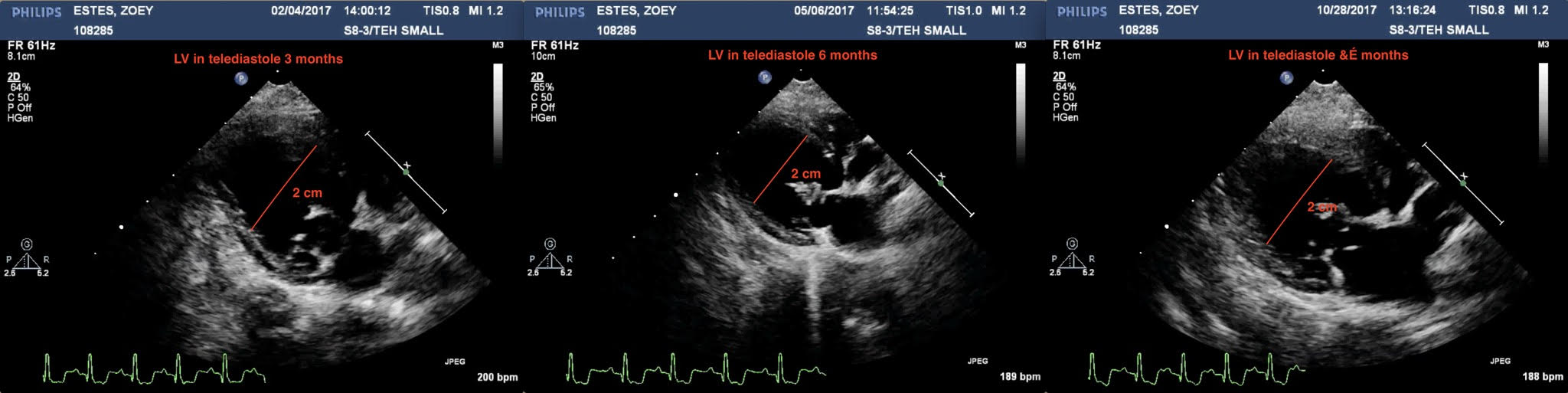
The 2nd reconstruction is of the long axis LV diameters in telediastole at 3-6-12 months. They measured 2, 2 and 2 cm = same.
Echocardiograms showing Left Ventricle (LV) measurements at 3 months, 6 months, and 12 months post operatively
The 3rd reconstruction is of the long axis view of the mitral regurgitation color flow map at 3-6-12 months = same ; so there isn’t any chance for the LA pressure to increase considering that the 12-month MR is the same as the 3 month and the 6 month post-op checkups.
Echocardiograms showing regurgitation at 3 months, 6 months, and 12 months post operatively
This is the manner in which Dr. Sabine uses with Dr. Uechi to review the cases post-operatively.
Zoey with Dr. Timothy Hodge at UC Davis
It’s very important to note, all operators can cut a heart a little differently and measure slightly differently during the same examination or during different examinations a few months apart. Some other factors like Zoey's large pulmonary vein ostium can make the measurements difficult to compare. Also, after surgery, some hearts have mild different anatomy because of the sutures, or because it has possibly turned a little in the thorax etc... Zoey is doing very well and there is no need for concerns.
Zoey is still off all her medications and doing quite well. I write this in hopes you all understand how important it is to have the doctors review your records after each checkup and assess. My doctor wasn’t doing anything incorrect and I completely trust him. The surgery repair is just widely unknown and many don’t understand the long term results. As more of us return to the US with our babies we all can help play a vital role in educating everyone, awareness is very important.
Zoey with her favorite person on the planet, daddy Nate
Post-Op Activity
Remember that you have made an incredible journey by choosing open-heart surgery for your beloved dog, so please take care of the repaired valve as best as you can so that you can enjoy a lifetime with it!
Recommendations for Open-Heart Surgery Post-Operative Activity
The importance of post-surgery healing process
For the first, second- and third-month post-op, you would have been given guidelines by your surgery team on what to avoid, what movement is acceptable and how much exercise your dog is recommended. It’s vital that given guidelines are followed to allow a successful healing process to take place.
The first three months is the most crucial time in the healing process as the heart is remodeling itself. By helping your dog to eliminate certain movement you are supporting the foundations for a stronger healthier heart muscle. It is therefore essential that certain movement is avoided or eliminated from daily life and activities. By planning, preparing and preempting situations, you will make way for a successful healing process. This is not to take place of the advice of your dog’s Cardiologist.
Surgery recovery postop month 1-3
•Patients should be kept under strict rest.•No jumping up / No jumping down•No stairs•No abrupt starts and stops.•Please keep your pets separated from other animals in the home. This will avoidplay and other movement that may disrupt healing of repair.•Set up a pen area as this is a great way to keep dog at rest. This will ensure thedog stays calm and resting when you are not around.•Block off furniture - Please keep dog off bed/sofa, so your dog is not tempted tojump off.
Shampoo or grooming
• No shampoo until 1month post-surgery.
• If skin/hair gets dirty, you may wipe him/her down with a wet towel.
Walking instructions
• Specific instructions may be given depending on your dog’s post-op condition.
After 3 months:
• keep dog on leash (even when in yard/garden/walks)
• Allow dogs to meet and greet in controlled environment.
• Begin walking your dog, on lead for 20-30 minutes twice per day.
• No running
• No Jumping
• No stairs
• No abrupt starts and stops.
• Please continue to keep dog off bed/sofa, do not allow them to jump off anyfurniture.
• No frantic play, No zoomies, no chasing wildlife, or animals
• You can allow gentle play interaction with other dogs.
After 6 months
• Please continue to keep your dogs on lead during this time, due to risk of high energy play with other dogs.
• After 6 months, you may use a ramp when needed, in place of stairs.
• No wildlife and/or animal chases, avoid high energy play, avoid high energy dog sports such as agility.
Remember that you have made an incredible journey by choosing open-heart surgery for your beloved dog, so please take care of the repaired valve as best as you can so that you can enjoy quality time with your pup!
Please contact your surgical clinic for the latest updates in post-op care or if you have additional questions
The Mighty Hearts Project team
Moni and Prudence
Levi's Surgery Story
The biggest unexpected surprise for our family came in July of 2016, when we took Levi in for a routine physical exam prior to having his teeth cleaned. Dogs have to go under anesthesia to have their teeth cleaned, and Levi has traditionally had some issues related to anesthesia and we wanted to be safe. His last checkup was in April 2016; he went in for an ear infection and at that time, he was in perfect health (except for the ear infection, of course). So it came as quite a shock when the vet announced that he heard a heart murmur level 4/5 for the first time in Levi's life...
Kim, Ginny, and Levi. Photo taken by Carolyn Scott Photography
The biggest unexpected surprise for our family came in July of 2016, when we took Levi in for a routine physical exam prior to having his teeth cleaned. Dogs have to go under anesthesia to have their teeth cleaned, and Levi has traditionally had some issues related to anesthesia and we wanted to be safe. His last checkup was in April 2016; he went in for an ear infection and at that time, he was in perfect health (except for the ear infection, of course). So it came as quite a shock when the vet announced that he heard a heart murmur level 4/5 for the first time in Levi's life.
A lot of small dogs develop a gradual heart murmur that starts low and builds as the dog gets older. We would not have been surprised if, at 9 years of age, that Levi had a minor heart murmur. But to go from zero murmur in April to a level 4/5 in July is alarming.
Heart murmurs in dogs can occur for many reasons, but the most typical of which is degenerative mitral valve regurgitation. The mitral valve is a flap in the heart that allows blood to pump into the ventricle, but not backwards towards the lungs. As a valve should work, it allows one-way movement. Degenerative mitral valve disease causes the thickening of the valve to the point at which it does not close properly and blood moves back and forth ineffectively in the heart. In response, the heart enlarges to allow for a larger capacity of blood pooling and to keep blood pressure in the body stable. Eventually, the excess fluid will back up into the lungs causing congestive heart failure.
We went to the cardiologist at the earliest possible moment. He confirmed that Levi did indeed have a level 5 murmur caused by degenerative mitral valve disease exacerbated by a chordae tendonae rupture. There are chords in the heart (literally what country singers croon about when they sing about heartstrings) that help coordinate the movement of the mitral valve flaps. If they break, the effectiveness of the valve is compromised significantly. That explains why it was not a gradual increase in murmur grade, but all at once.
We were devastated by the news, and we were further shocked when we were told that Levi had 6-9 months before he experienced congestive heart failure, and possibly a year left to live. We left with this news heavy in our hearts. Our devastation turned to anger and frustration. Why is there nothing that anyone can do to correct this issue in dogs? Humans have open heart surgery to repair the heart valves all the time - it's practically routine!
We emailed veterinarians at UC Davis, Cornell University, and several other highly respected veterinary schools in the US, along with one point of contact we found for veterinary surgeons in France. We heard back from the French doctors - they asked for more information about Levi and his results from our cardiologist.
We sent them, and held our breath.
We found more information about the doctors in France, and other dogs and owners from the US who had gone there to have the repair done. We called. We coordinated. We kept researching. No veterinary team in the US performs this procedure. Only one surgeon in the world - renowned Japanese surgeon named Dr. Masami Uechi - performs these operations currently in Japan, Singapore, and France.
Levi was in the loving care of Dr. Jean-Hugues Bozon and Dr. Sabine Bozon during his surgery and recovery
When we finally got word from the Clinique Veterinaire Bozon in Versailles, France that Levi was a candidate, we were still in a little bit of disbelief that this was possible, that this was actually something that we could and possibly WOULD do. Were we crazy? Would other people think we were crazy? Can we logistically pull this off?
Maybe we are crazy, maybe we just love our dog. We stopped caring what anyone thought of what we were doing. And yes, we logistically pulled it off . . . one day at a time, one piece at a time, one foot in front of the other. When you want to do something that seems impossible in foresight (and hindsight), you have to know that the little steps in between to make it happen just come as long as you keep moving. We never lost faith, even when it was tested over and over again. I was taught that my heart and my hope are infinitely bigger than I ever realized.
It was unexpected. All of it. The diagnosis. The plan of action. Even the result.
Levi with Dr. Neal Peckens at CVCA
We expected resistance and judgement anytime we talked about cardio-pulmonary bypass surgery for our dog . . . in FRANCE. But, everywhere we turned, friends and family knew exactly what Levi meant to us, and agreed we were doing the right thing for him. Our vets Dr. Carole Richards and Dr. Chris Vanderhoof at Caring Hands Animal Hospital, and Dr. Neal Peckens at CVCA, were 100% on board with us when we made the decision to go forward with it. They ran tests, and re-ran tests, and asked questions, and cared for us as owners. They cheered us on, and helped Levi recover when we got back.
We knew before we even went to France for the surgery, before we even knew Levi would live through it, that we wanted to be of service to Dr. Sabine and Jean-Hugues Bozon. We didn't know how, but we felt so inspired by what they are doing. When we met them, saw their clear vision of the future, learned about the many leaps of faith they took to get where they are, and witnessed the loving care they put into every living being that they touch, it was very clear to us and a few owners who came before, that we would need to take our own leap of faith to help them, and to help this cause in some way. And that is one of many reasons that Mighty Hearts Project was born.
Though most of all, it was unexpected what two people with love and hope in their hearts can accomplish together. I do mean Ginny and myself; however, we saw it in Dr. Sabine and Jean-Hugues as well. Their love for each other and their love for saving animals is unparalleled. Dr. Sabine taught us not to ever lose faith in something that is important to you. If the solutions presented to you are unacceptable, find new solutions.
We are currently on a mission to find new solutions for dogs in the United States. We will not lose faith.
Levi, sitting up in his oxygen recovery cage just a few hours after his mitral valve repair surgery at Clinique Veterinaire Bozon in Versailles, France
The LOOK Study: ACVIM Conference 2017
The Longitudinal Outcome of Canine Mitral Valve Disease (LOOK-mitral) - by Dr. Michele Borgarelli, DVM, PhD, DECVIM-CA
This is a study being performed with the collaboration of Virginia-Maryland College of Veterinary Medicine, where Dr. Borgarelli does his research, and one of the largest veterinary cardiology practices in the United States, CVCA. The purpose of the study is to assess the natural history of mitral valve disease (MVD) in a large referred population of dogs, assess the prevalence and effects of co-morbidities on the natural history of the disease, and to identify risk factors for progression and death.
The Longitudinal Outcome of Canine Mitral Valve Disease (LOOK-mitral) - by Dr. Michele Borgarelli, DVM, PhD, DECVIM-CA
This is a study being performed with the collaboration of Virginia-Maryland College of Veterinary Medicine, where Dr. Borgarelli does his research, and one of the largest veterinary cardiology practices in the United States, CVCA. The purpose of the study is to assess the natural history of mitral valve disease (MVD) in a large referred population of dogs, assess the prevalence and effects of co-morbidities on the natural history of the disease, and to identify risk factors for progression and death. Collected data includes physical exam, radiographic findings, ECG findings, presence of co-morbidity, laboratory results and treatments.
Since October 2015, vets from CVCA have been submitting information from a large population of dogs with MVD to the LOOK Study. This is strictly an observational study. Inclusion criteria for study enrollment is a diagnosis of MVD confirmed by echocardiographic exam. Dogs are enrolled in the study at the time the diagnosis is confirmed by a cardiology specialist. 2,053 dogs have been observed as of April 30, 2017, and new dogs can continue to be submitted to the study until September 2017. Data on the dogs enrolled in the study will continue to be collected until it concludes in October 2020 or until the death of the dog.
The current population of dogs in the study represent 104 different breeds. The largest segment being mixed breed at more than 300 dogs, second highest is CKC, then Chihuahua. 48% of dogs are female, and 52% are male, and for both male and female, approximately 90% are neutered/spayed. The median age of all dogs is 10.3 years, but it was noted that the average age for the CKC is much younger than the median.
57% are Stage B (75% of which are B1, 25% are B2), 39% are Stage C, and 4% are Stage D. During the current 20 months of the study, only 4.5% of dogs have passed. It was noted that this could be because most dogs being submitted to the study were new cases presented at CVCA which typically occur at the earlier stages.
Some of the preliminary findings of the study so far are:
- Echocardiogram results are more important than the observation of a heart murmur, as more than 4% of dogs with the disease had zero murmur. In high risk breeds, this suggests that regular preventative cardiology exams with echocardiogram are warranted rather than waiting until the onset of symptoms.
- Nearly 80% of dogs are referred to cardiologists due to the presence of a cough.
- Most concomitant disease is chronic respiratory disease.
Additionally, at the conclusion of the conference session, Mighty Hearts Project participants were able to inquire with Dr. Borgarelli on whether dogs who have had an intervention, such as Dr. Uechi's Mitral Valve Repair surgery, were noted and being tracked within the study with this information in mind. Dr. Borgarelli confirmed that is correct. One dog that we know of being tracked as part of the LOOK study is Levi, who has had a successful mitral valve repair since his initial diagnosis. Levi is seen by Dr. Neal Peckens at CVCA in Virginia.
Mitral Valve Repair Metrics
One of the most frequent questions asked when considering a surgery as risky as cardio-pulmonary bypass, is what are the chances my dog will survive the surgery and what is the long term prognosis post-surgery. The answer is always "it depends". Each dog is different, and each circumstance is unique. Below are some guidelines to help you determine the best course of action for your dog based on aggregate data. For more specific recommendations regarding surgery for your dog, please contact Clinique Veterinary Bozon or JASMINE Veterinary Medical Center directly. Additional mitral valve repair statistics may be found in an abstract published by Dr. Masami Uechi from October 2016.
One of the most frequent questions asked when considering a surgery as risky as cardio-pulmonary bypass, is what are the chances my dog will survive the surgery and what is the long term prognosis post-surgery. The answer is always "it depends". Each dog is different, and each circumstance is unique. Below are some guidelines to help you determine the best course of action for your dog based on aggregate data. For more specific recommendations regarding surgery for your dog, please contact JASMINE Veterinary Medical Center directly. Additional mitral valve repair statistics may be found in an abstract published by Dr. Masami Uechi from October 2016.
Global survival rates of dogs who have undergone Mitral Valve Repair with Dr. Masami Uechi:
99% in stage B2
95% in stage C (if no pulmonary hypertension (PHT) before surgery)
85% in stage C (if there is PHT before surgery)
75% in stage D
The younger the dog is, the higher the success rate.
80% of the dogs operated on do not need any treatment or additional medications for mitral valve disease after surgery.
Mitral valve repair is needed if one or more of these conditions are present:
If the dog is 13 years old or less AND
As soon as the dog is in stage C
If there is chordae tendinae rupture and/or grade 3 prolapse (even in stage B2)
If there is a grade 3 or 4 mitral regurgitation (even in stage B2)
If pulmonary arterial pressure (PAP) is less than 50 mmHg (otherwise the dog must be put on sildenafil 1-2 months before surgery)
If the 2D LA/AO ratio in SAX is > 1.6 (right parasternal) (The LA/AO - meaning Left Atrial to Aorta Ratio - uses the relatively fixed diameter of the aorta to assess the degree of left atrial volume loading)
If the NT-ProBNP level is > 2100 mol/l (even in stage B2)
Mitral Valve Repair under Cardio-Pulmonary Bypass (CPB) is a very complicated procedure
Weak points triggering a poor recovery from CPB are:
The age of the dog (older dogs are more prone to Systemic Inflammatory Response Syndrome and thrombosis after surgery because their endothelium is more damaged)
The degree of PHT before surgery (because one of the side effects of CPB is PHT)
The systolic/myocardial function (because there is myocardial ischemia during CPB and the recovery is directly related to the myocardial health before surgery)
The severity of the ACVIM stage
The surgery might be contraindicated (or have a lower survival rate) if:
The dog is more than 13 years old
There is severe PAP not improved after sildenafil therapy
There is myocardial dysfunction/ischemia (low cardiac output) before surgery
There is any concomitant medical disease (a secondary illness), for example:
A neoplastic process (a mass or tumor)
everely impaired renal function such as nephrotic syndrome or protein-losing enteropathy (kidney disorders)
Severe hepatic insufficiency (liver failure)
Unresolved infections
ndocrine disease (such as Cushings)
Hypothyroidism can be adjusted and treated 2-3 months before surgery
There is coagulation dysfunction (an issue with blood clotting) and especially decreased levels of antithrombin 3 before surgery
Surgery might be difficult if there is a significant aortic insufficiency, an observation that must be recorded in the cardiology report