Mitral Valve Repair Intervention Explained
This is not a simple surgical procedure. It is a complete and very complex medical-surgical procedure from the preoperative phase to the hospital discharge 7-10 days later, where a team of 10 veterinarians intervene for a single dog. Each veterinarian has a specific role, either medical or surgical. The procedure requires 2 surgeons (surgeon and one assistant surgeon), 3 sterile instrumentalists, 3 non-sterile assistants, 1 perfusionist, 1 anesthetist-resuscitator, and 1 cardiologist sonographer.
Here we will break down some of the processes of this procedure to give you a broad understanding of this complex intervention.
“The success of this intervention is due to the perfect harmony of a team that is perfectly in sync together where everyone has his or her designed roles, no technical details are left to chance.”
The “master machine” that makes open heart surgery possible is called the Cardio-Pulmonary Bypass (CPB) Machine. In addition to this machine, the intervention requires 2 anesthetic machines - one with assisted ventilation (isoflurane or sevoflurane), a monitor to show live vital statistics, a thermal generator which cools or reheats the animal’s body on request at a precise temperature, a surgical table inclinable in all directions, an echograph with color doppler and a pediatric transesophageal probe, 4 syringe pumps and 2 infusion pumps, a coagulation time measuring device, a blood gas analyzer, a blood-biochemical analyzer, an electrolyte analyzer, an internal pediatric pallet defibrillator, a pace-maker, fresh blood compatible for transfusion (a machine called “cell-saver” in order to recycle the lost blood and carry out autotransfusions), a cardioplegic solution (which stops the heart), frozen sterile physiological serum, a large number of consumables and injectable medicines, conventional surgical aspirator equipment, a fine-tuned electric scalpel, microsurgical instruments, customized equipment (catheter, tubing, etc…) and more.
Extracorporeal Circulation
“This is one of the biggest constraints of the intervention for small breeds dogs. With special modifications They are able to operate on dogs weighing 2kg or less. Extracorporeal circulation techniques have been attempted in some medium or large sized dogs before without huge success”
In dogs of any small size, difficulties are encountered given the low initial circulating blood volume. Dr. Uechi has succeeded in developing an extracorporeal circulation procedure that does not use traditional techniques, and allows the operation of miniature dogs and even cats. The use of extra-corporeal circulation can induce cardiac arrest and therefore work freely for the time required during the surgical open heart repair.
The CPB machine allows the heart and lungs to be taken over during surgery and requires: 3 pumps (one of which is equivalent to the heart pump), a system for mixing and exchanging blood cases (oxygenator, equivalent to the lungs), a system for controlling blood and body temperature (thermal generator), a tubing system adapted to the conformation of the dog. The mastery of extracorporeal circulation by the perfusionist is crucial to the success of the intervention. Mastering extracorporeal circulation is the future in terms of treatment of heart disease in dogs.
Steps of the Surgery
Prior to the induction of general anesthesia, the maximum number of steps is performed on animal vigil: insertion of 2 intravenous catheters (typically in anterior limbs), insertion of a urinary catheter (Foley catheter), shaving the left cervical area, the entire left chest wall, and the medial right posterior limb. The operating room is also prepared during this phase.
Premedication
General anesthesia
Surgical placement of an arterial catheter and venous catheter to measure invasive arterial blood pressure and central venous pressure throughout the procedure and especially during cardiotomy (heart stopping phase, approximately 2 hours).
Surgical opening of the rib cage, reclination of the lungs, pericardiectomy and access to the heart.
Dissection of the base of the aorta and minimal separation of the aorta and the pulmonary artery.
Administration of intravenous bolus heparin to induce a non-coagulable state. For this purpose, measurements of the activated partial thromboplastin time (ACT) are carried out until a minimum value of 300 seconds is obtained.
Laying of extracorporeal circulation cannulas. The left carotid artery and jugular vein are surgically isolated and a cannula is inserted into each vessel, their size depending on the type of cannulated vessel and the body weight of the dog.
Implementation of the partial and then total extracorporeal circulation. The cannulas are connected to the extracorporeal circulation circuit after carefully evacuating the air bubbles from the tubing. The arterial and venous lines are unclamped and the CPB starts at the adapted rate.
Transesophageal ultrasound: a pediatric transesophageal tube connected to an echocardiograph equipped with color flow doppler is inserted delicately in order to successfully obtain the median transverse and longitudinal views. The movement of the mitral leaflets and regurgitation are examined by the surgeon.
Catheterization of the ascending aorta (installation of the cardioplegia cannula): a catheter is gently inserted on the left lateral face of the ascending aorta.
Decreased body temperature: the body temperature is gradually decreased up to 28 degrees and maintained thanks to the thermal generator integrated in the extracorporeal circulation machine.
Injection of cardioplegic solution (via blood cardioplegia) in the coronary arteries via the aortic catheter and induction of cardiac arrest.
Incision of the left atrium and placement of the aspirations cannulas.
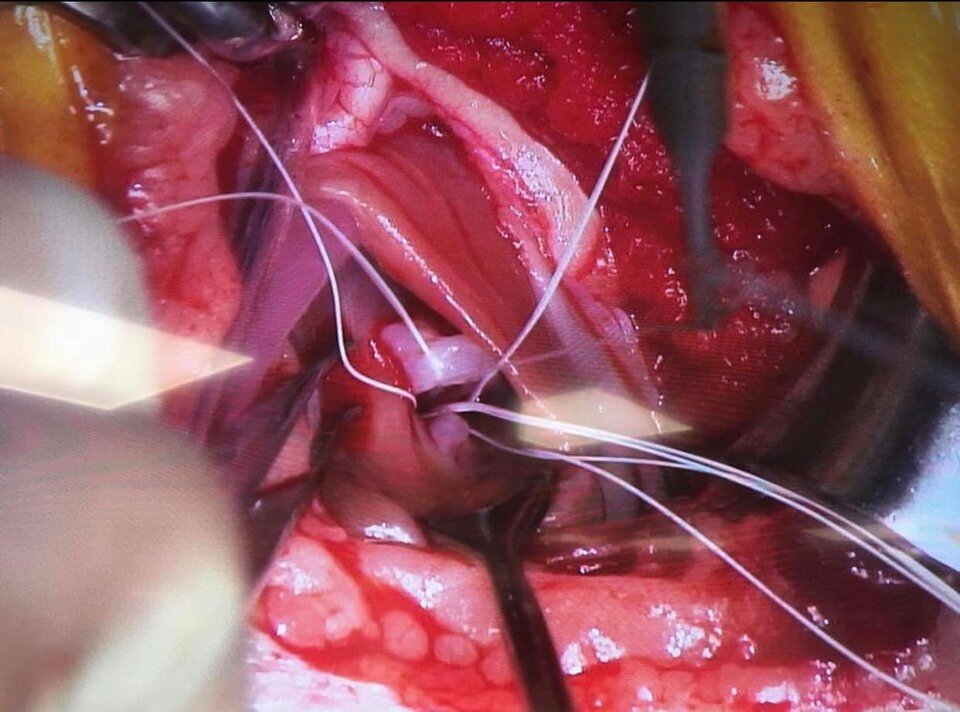
Pre-placement of artificial cordage’s: replacement of mitral tendon cords is the best technique for repairing broken cords. Double sutures of expanded polytetrafluoroethylene (e-PTFE or Gore-Tex) are placed between the papillary muscles (reinforced by pledgets to avoid tearing of the papillary muscle) and the mitral leaflets. Depending on the dog, a total of 4 to 6 new cords are laid.
Mitral annuloplasty: tightens the mitral ring in order to decrease or even cancel the mitral regurgitation and thus to maintain a good systolic coaptation. The same material as the cords is used (ePTFE) in the form of two sutures reinforced by pledgets at the level of each commissure of the mitral ring.
Tightening of the replacement cords: the main challenge here is the difficulty in adjusting the cords, in length and tension, in order to obtain the optimum coaptation when closing the mitral valve. This phase is highly dependent on the surgeon’s experience and the mitral valve leaflets echostructure. The result is then tested with physiological serum under pressure in the left ventricular chamber by tilting the table.
Suture of the left atrium, evacuation of the intra-atrial air under transesophageal ultrasound control and declamping of the aorta.
Restarting the heartbeat: upon cessation of intracoronary administration of the cardioplegic solution, heartbeats are expected to resume spontaneously. A direct cardiac massage is performed systematically and if the heart does not restart on its own, a temporary pacemaker is placed or ventricular defibrillation is undertaken.
Transesophageal ultrasound recheck: the coaptation of the mitral leaflets and the mitral regurgitation are appreciated, which has usually decreased by at least 80%.
Progressive temperature rise in the body of the animal and gradual decrease in the flow rate of the arterial pump.
Removal of the carotid and jugular cannulas and termination of the CPB.
Continuous perfusion of protamine (heparin antagonist) over a 20-minute period. Simultaneous administration of continuous dobutamine infusion if invasive blood pressure is too low and unstable. Indeed, protamine can cause severe hypotension, bronchospasm and increased pulmonary vascular resistance. Ventilation and blood pressure should therefore be perfectly controlled at this time.
Closure of the thorax plane by plane (the pericardium is not sutured).
Chest tube placement.
Progressive waking over 2-3 hours: During this crucial phase, all the vital parameters and ventilation are closely controlled and their return to normal are obtained very gradually. Femoral catheters will be removed just before the actual wake-up (isoflurane stop) once invasive systolic blood pressure remains stable. The dog is then placed in an intensive care cage with oxygen supply and regulation of the ambient temperature as well as hygrometry.
Example pre-placement of artificial cordage’s
Postoperative Care and Prognosis
Once the mitral valve is repaired and the new cords are laid, the mitral prolapse improves, the coaptation of the leaflets are almost normalized and the mitral regurgitation is decreased by at least 80% in most dogs. There is incredible plasticity of the left atrium which has the ability to shrink back to its normal size in less than a week if the quality of the muscle will allow it. On the other hand, the treatment for heart failure is either stopped the day after the intervention or gradually over a period of a month.
Some dogs require ongoing further treatment if the repair was very difficult, however most only require blood thinners prescribed for 3 months. This is to prevent thromboembolism (blood clotting), the most frequent complication seen postoperatively, the maximal risk being between the 1st and 4th days after surgery but can last longer especially in Cavalier King Charles Spaniel breeds.
Some cases of acute pancreatitis have also been seen postoperatively, follow-up of specific pancreatic lipase is recommended during the week of hospitalization. A systemic inflammatory syndrome is more or less always present and must be managed, as best as possible.
Operating theater at the Jasmine Clinic in Japan
After the procedure, “the goal is for the dog to recover to a life of an asymptomatic dog in the early stages of the disease before going into heart failure requiring almost no treatment for congestive heart failure, including medications such as furosemide for most of them depending on the heart damage before the surgery, even if they were in stage D before surgery.”
Consequently, it is the hope most dogs who have received surgical intervention no longer suffer from respiratory problems, regain the possibility of exerting effort, regain appetite, regrow, or no longer suffer from kidney failure. If treatment persists, it is sildenafil which is still necessary in half of the dogs who had pulmonary arterial hypertension prior to surgery.
It is possible to operate at any age, but before 13 years is the most ideal. A complete medical and biological check-up must be carried out before each surgical intervention so that no other accompanying illnesses will cloud the prognosis. The surgical procedure (induction of anesthesia until closure of the thorax) usually lasts from 4 to 8 hours depending on the complexity of the case.
It takes 2 hours of preparation to gather all of the materials needed for surgery as well as preparing your dog before the anesthesia and 3 hours of progressive awakening after they are removed from the bypass machine and the thorax is closed and they are eventually moved to recovery. The entire procedure end-to-end lasts 9 to 13 hours, depending on the case.
Hospitalization is required for 1 week after surgery. A thoracic drain is placed at the end of surgery and typically removed the next day. The dog can stand the day after surgery and can drink water and eat a little. A continuous infusion of Fentanyl (pain medication similar to Morphine) is administered the day of and the day after surgery unless needed longer. The surgery is not painful.
During the week of hospitalization, dogs are monitored hourly, vital parameters are tracked, solid food is administered, echocardiogram and a doppler is performed at least once daily. Ventricular arrhythmias are frequent in the first postoperative days. They very rarely require further ongoing treatment with medications and disappear spontaneously and gradually during the first week.
A week after surgery, the dog is only allowed to go out for brief, slow walks for about a month, and modified resumption of physical exercise is allowed after 3 months.
Please see this article posted about post-operative physical activity recommendations for more important aftercare information.
Mitral Valve Surgical Treatment Corrects a Mechanical Defect
Surgical treatment corrects the mechanical defect while medical treatment can only mitigate the negative consequences of mitral regurgitation. The surgical technique was developed over 12 years ago at the Nihon University by Dr. Masami Uechi. This technique reduces the diameter of the mitral ring, called annuloplasty, to significantly reduce mitral regurgitation and replaces cords to avoid mitral valve prolapse. This surgery is still carried out to date with a (Discharge) rate of about 97%. Dr. Masami and his team at the Jasmine clinic in Yokohama Japan continue to improve upon that number.
“Dr. Uechi is the most experienced canine mitral valve repair surgeon in the world today, and has already operated on thousands of dogs.” His strength is his ability to be both a veterinarian doctor and a surgeon. He began his career as a professor of internal medicine in cardiology and nephrology. After seeing so many dogs with mitral valve disease (MVD) dying from kidney failure as a result of suffering from heart failure (CHF) under high doses of furosemide (a diuretic commonly known as Lasix in the United States), he directed his research towards surgical cardiology because he wanted to do more for them besides medication management.
Frustrated with so few available medical surgical treatments, Dr. Uechi decided to tackle this cause, relentlessly trying to repair the degenerative mitral valve and broken tendon cords. His goal was to wean the dogs off from their current treatments by repairing the mitral valve in return lengthening their life expectancies inherent to their breeds.
Still surrounded by a few students who were part of his initial team, Dr. Uechi, who was an internist, gradually became a surgeon where he successfully succeeded in finalizing this procedure after 7 years of dedicated work before finally publishing it in the Journal of Veterinary Cardiology in 2012, only after he was satisfied with the rate of success.
Faced with the high success of his new procedure, Dr. Uechi left the university and established his own clinic (Jasmine) which is a referral type structure specifically dedicated to this cardiac surgery under extracorporeal circulation. As the leader and pioneer of mitral valve surgical repair on canines, Dr. Uechi has built and educated a team of phenomenal veterinarians at his Jasmine clinic where they currently are performing up to 6-9 surgeries a week.
Each team member performs his/her role to complete perfection. It is a result of their individual mastery of each specialty skill required in order to achieve this, these skills for example are: Extracorporeal Circulation (crucial point), Anesthesia and Resuscitation techniques, Postoperative 24 hour intensive care, Cardiology, Doppler Echocardiography, and finally the surgical repair technique.
Dr. Uechi is currently the only one to be able to successfully make a hand-made repair of the mitral valve during the crucial phase of cardiac arrest. Not many human cardiac surgeons use this repair technique which is the gold-standard treatment. They would rather use the mitral valve replacement technique, which lasts for only approximately 10 years, by suturing a pre-prepared annulus which is much easier and faster to perform than the made-to-measure repair.
In small breed dogs, it is even more difficult technically speaking and, unfortunately, a replacement is impossible in dogs because they do not have the same coagulation system as humans and such a small size artificial annulus does not exist to date for canines.
A pre-surgical screening tests by your veterinarian must be taken before proposing such an intervention to an owner, the clinics performing the mitral valve repair procedure will assess the medical data and advise you if your dog is a suitable candidate. It is important to give owners some time for reflection after hearing all the possible surgical complication risks, as it is a significant psychological and financial investment.
Nevertheless, this new procedure is a real revolution in the treatment of canine heart disease. We hope it will be carried out routinely in the next 10 years in some specialized centers. This is a very complex procedure and requires the strict attention to details in order to achieve the highest possible success rates. For this, the conditions must be optimal at the human and technical level. Nothing should be left to chance. Please visit our Resource page, (travel to) sections to find the contact information for each center we support.
For more questions about the repair surgery, please visit our FAQ page.